A month ago was my third heart surgery of the summer. It's hard to actually keep it all straight. In April my arrhythmia went off the rails and didn't come back on - it started with an ER visit at GW while I was in D.C. for work and never really right-sized. We tried three different anti-arrhythmic meds and a couple of beta blockers but none of them suppressed my arrhythmia and the side effects were awful. Having failed medical management, I had my first surgery on June 3rd. They did about an hour of pacing and most of the EP study, but had given me anesthesia that suppressed the PVCs so they weren't able to do the actual ablation. I woke up in the OR to them telling me they weren't able to do the ablation, which was awful. Two weeks later I went back on June 18th but had no active arrhythmia and never made it back to the OR. At the time, my arrhythmia was bigeminy, which you can't induce - it has to be active at the time of surgery or they won't be able to map where to ablate. Two weeks later I went back and had my second surgery and first "successful" ablation on July 1. I'd had an arrhythmia the whole pre-op period (for hours) and when I went back to the OR, it stopped. Dr. Moore decided to try slowing my heart rate down to see if that would make it kick back in, and it did. After giving me a big dose of metoprolol, I ended up in bigeminy and we were able to do the surgery. Because of the first failed attempt, I wasn't able to have anesthesia and only had light sedation during the ablations, so was awake for almost four hours of heart surgery (...wild). They did a lot of mapping and pacing but at the end of the 4 hours, I was still throwing PVCs in the OR. Dr. Moore decided to call it- hopeful that she had gotten the worst of it but not wanting to keep pushing the procedure at that point. After three hours of bed rest, the nurse helped me stand up and asked me to walk around my hospital room. After a few steps, I noticed drops of bright red blood on the floor and then there was a gush and blood pouring down my right leg- I was having a femoral artery bleed from where they'd gone in with the catheter. So that was some excitement - a code team and some anxious watching and waiting, but everything ended up okay (I still owe the very young nurse who kept her body weight on my artery for 40 minutes a bottle of Malibu rum). My arrhythmia was awful through the night, but I was told it could take up to 3 months to notice a difference and to not worry. After a week it was still terrible, and then about six days after surgery I ended up with terrible chest pain and was diagnosed with pericarditis. I started medication and one week later, woke up feeling like I had turned the corner. I actually foolishly told people I thought I was doing better. That night, I ended up with a weird feeling in my chest that was different, and shooting pain under my left should blade and down my arms. The "episodes" were lasting about 45 seconds, and on about the 3rd one I felt myself lose my breath and had to lean against a wall and lower myself to the ground. When I got to the ER, I told the person who was taking me back that I thought when they put me on a monitor I'd be tachycardic (and was thinking it was a complication of the pericarditis). Turns out- it was a new arrhythmia- ventricular tachycardia. My HR was around 200 without perfusing blood for 30-60 second runs. They moved me to the stablization room and put defibrillator pads on my chest and back and started an amiodarone infusion- the ER docs didn't know if I had the type of VT that converts to Vfib- but told me I wouldn't die now that I had the defibrillator pads on (not the most comforting thing to be told). I was admitted to the cardiac ICU and spent the night not knowing what kind of VT I had- mostly thinking about the boys. Tuesday morning I met my new cardiologist who told me I have idiopathic VT (not the scary kind that kills you) and that eventually I would need surgery again but that with active pericardits and being so close to the last surgery the goal was to get me on the oral version of the infusion and send me home for a few weeks before coming back for surgery. I was so happy- that was the best news. I was able to eat (I'd been NPO when they didn't know if I needed surgery) and was planning to go home that day. But as soon as they took me off the infusion, things went wild. I had back to back VT runs for an hour, almost losing consciousness a couple of times, before they called it and put me back on the infusion. No going home- I would need to have surgery the next day. On July 17th I had my third surgery. When I got to the OR, I wasn't having the VT and the surgeon gave me the spheel about needing to have an active arrhythmia to pace and map (though they'd captured the VT on a 12-lead and confirmed it was the same spot my previous surgeon had ablated based on her notes). They gave me 2 units of adrenaline and the VT kicked in right away, and we were off-- again no anesthesia, but also no sedation during the ablation. I felt all six burns, but on the plus side the team listened to Lady Gaga in the OR. Dr. Pham waited for over an hour after finishing the last ablation, increasing the adrenaline up to 10 units, without a single PVC. He was sure they'd gotten it- he'd done a heavy ablation on the spot, and then smaller burns around it to disrupt any "halo" effect of the bad circuit. He also shared that the spot he hit had no scarring- so would have been different than what they'd done previously. I left the OR thinking everything was done, and being so happy. Then at 12:15 a.m., I woke up to VT runs. They went on through the night, but they were short and weak, though still there. The docs think that means surgery didn't work and that I'll need a 4th surgery this fall. They described my heart as an angry tiger- that when they heat it, the arrhythmia goes dormant and is "stunned" but then wakes up later and is not happy. They restarted me on flecainide (the first anti-arrhythmic I had tried) and kept me another night to make sure it initiated okay (which it did). After 5 days in the ICU I got to go home on the 19th.
I haven't had a single PVC since 6 a.m. on July 18th. I think surgery actually worked, but we will see when I eventually try coming off the med. I feel pretty good now- some lingering pain in my arm from one of the infusion sites and in my groin (they went in through the same arteries and veins for all three surgeries - eight catheters in total- so that will probably take a while to bounce back from). I'm staying away from caffeine and alcohol and took June-August off of air travel, but in September things pick up so we'll see how it all holds.
All in all, I feel incredibly lucky. It was an unexpectedly hard and painful summer but at the end of the day, I am healthy and healing and will be okay. Thank you to everyone who helped me 💗
Heading to the first surgery
Blood pressure in pre-op before surgery #1 was 78/58... what could go wrong?
Failed attempt...
2nd surgery
Rhythm strip the day of surgery
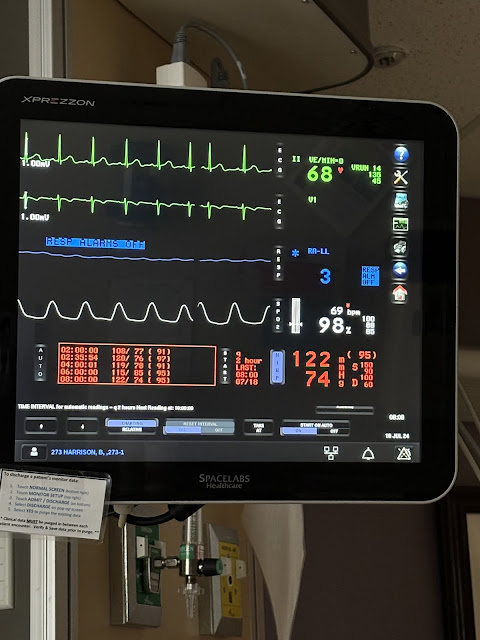
3rd surgery- VT
What VT looks like on a monitor
(Compared to beautifully normal the day I left the ICU)
New accessory- difibrillator- stayed on for 2 days
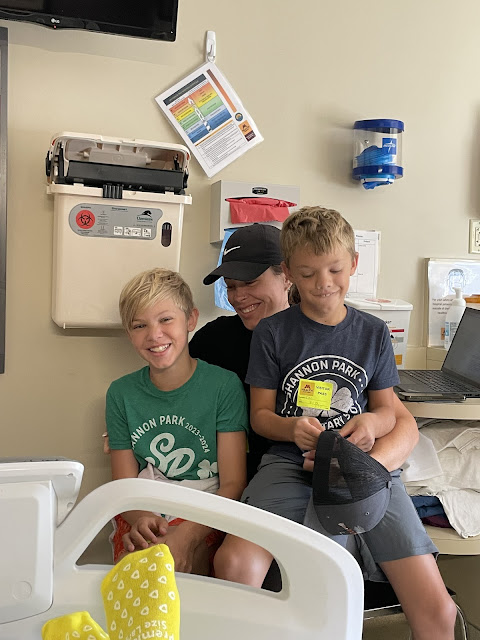
Getting ready for the boys visit before surgery- trying to hide all the IVs and wires
Boys visit after surgery
Watch dog.
Leaving the hospital




















No comments:
Post a Comment